- Home
- About
- Partners
- Newcastle University
- University of L'Aquila
- University of Manchester
- Alacris Teranostics GmbH
- University of Pavia
- Polygene
- Consiglio Nazionale delle Ricerche
- INSERM
- Certus Technology
- Charité Universitaet Medizin
- GATC Biotech
- University Medical Center Hamburg Eppendorf
- Evercyte GmbH
- University Hospital of Cologne
- PRIMM Srl
- University of Freiburg
- University of Antwerp
- Finovatis
- Research
- SYBIL at a glance
- Bone
- Growth plate
- Desbuquois dysplasia
- Diastrophic dysplasia
- MCDS
- Osteopetrosis
- Osteoporosis
- Osteogenesis imperfecta
- Prolidase deficiency
- PSACH and MED
- Systems biology
- SOPs
- Alcian Blue staining
- Bone measurements
- BrdU labelling
- Cell counting using ImageJ
- Chondrocyte extraction
- Cre genotyping protocol
- DMMB assay for sulphated proteoglycans
- Densitometry using ImageJ
- Double immunofluorescence
- Electron microscopy of cartilage - sample prep
- Extracting DNA for genotyping
- Grip strength measurement
- Histomorphometry on unon-decalcified bone samples
- Immunocytochemistry
- Immunofluorescence
- Immunohistochemistry
- Quantitative X-ray imaging on bones using Faxitron and ImageJ
- Skeletal preps
- TUNEL assay (Dead End Fluorimetric Kit, Promega)
- Toluidine Blue staining
- Toluidine Blue staining
- Von Kossa Gieson staining
- Wax embedding of cartilage tissue
- Contact Us
- News & Events
- Links
- Portal
Bone
Human skeleton consists of 206 bones, providing scaffolding for other organs and connected to the rest of the tissues via the network of cartilage, tendons and ligaments. Bone is a dynamic tissue, which is directly influenced by mechanical load as well as hormonal and signalling pathways and it acts as a reservoir of blood calcium in the body.
Bones form in two distinct ways, via intramembranous ossification (primarily the craniofacial skeleton) or via endochondral ossification (long bones in the body). Endochondral ossification involves a structure called the growth plate cartilage which is responsible for the longitudinal bone growth. Both ossification pathways are implicated in bone repair at later stages of life, with intramembranous ossification being the method of repair for stabilised fractures, whilst unstable fractures often heal via endochondral ossification.
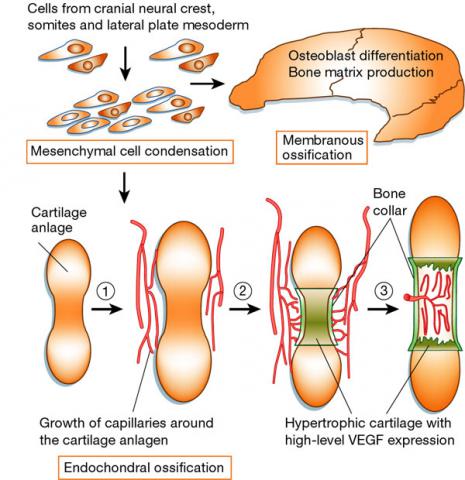
Zelzer&Olsen, Nature (2003) 423: 343-348
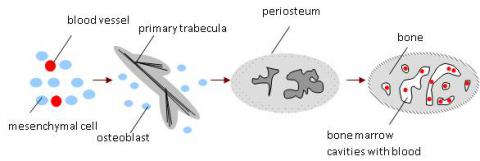
Intramembranous ossification begins with neural crest cells migrating, condensing and undergoing mesenchymal transformation. The number of blood vessels increases in spaces between the mesenchymal cells and the cells condense and start secreting extracellular matrix molecules, forming a condensed connective tissue membrane, which then differentiates to bone. Mesenchymal cells, in close proximity to blood vessels differentiate into bone forming cells called the osteoblasts. They start to secrete osteoid (ground substance), the organic bone component consisting mostly of collagen fibrils, which are laid down in long strands. Finally they begin to deposit calcium salts, thereby starting the mineralisation process. Osteoblasts then differentiate into osteocytes, which migrate to bone cavities and start to secrete hydroxyapatite, the inorganic component of the bone extracellular matrix. Trabecula (lat. little strand) is formed, consisting of osteocytes surrounded by mineralising osteoid, and then by osteoblasts forming a sheath around the structure. Trabeculae run in three dimensions, giving the bone a sponge structure and between them bone marrow cavities are formed. When the trabeculae contact each other a lattice structure forms. Osteocytes connect by cytoplasmatic extensions in the bone canals. During the process called appositional growth osteoblasts secrete new layers of osteoid and systematically differentiate into new osteocytes. Most bones are mixtures of two bone types, having compact outer surface and porous interior filled with bone marrow.
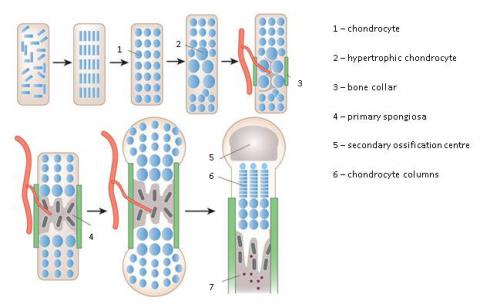
Endochondral ossification is primarily associated with long bone formation. At the start of this process, mesenchymal cells condense and migrate to the site of bone formation. Here they are induced to become chondrocytes, round cells secreting extracellular matrix primarily consisting of collagens and mucopolysaccarides, which then proliferate into a dense tissue devoid of blood vessels called cartilage. As the cartilage grows, the cells are forced apart by the extracellular matrix and become encapsulated in the thickening matrix in a process called interstitial growth. On the cartilage surface the mesenchymal cells differentiate into perichondrium. They also continue to secrete extracellular matrix and form more cartilage layers in a process called appositional growth. Perichondrium then undergoes vascularisation, which stimulates mesenchymal cells to differentiate into osteoblasts. Perichondrium is converted into periosteum, this process initiating an osseous cuff formation around the cartilage scaffold. Meanwhile, within the body of the cartilage, the encapsulated cells die due to their intensive growth and calcium salt deposition, and the matrix eventually erodes. The blood vessels invade the cartilage, bringing bone-forming cells, which differentiate into osteoblasts and the remaining strands of cartilage act as templates. They secrete additional extracellular matrix, that is subsequently calcified forming trabeculae, which can extend and fuse. Some of the trabeculae are resorbed by the osteoclasts forming a bone marrow cavity.
 adapted from Kronenberg, Nature (2003) 423: 332-336
adapted from Kronenberg, Nature (2003) 423: 332-336
As the bones continue to grow, a secondary ossification centre is established at the end of the bone. It is formed in a similar way to the primary centre, by cartilage undergoing the same process of hypertrophy, matrix mineralization, vascular invasion and finally bone matrix deposition. However, much less chondrocyte proliferation is observed, and the process appears to be mainly for the conversion of cartilage into bone. Between the shaft of the bone and the secondary ossification centre a cartilage growth plate is formed, allowing longitudinal bone growth. The thickening of bone is achieved by depositing further layers on the periosteum side by osteoblasts, and widening of the bone marrow cavity by osteoclasts. Eventually, the two bone elements fuse, forming mature bone. Endochondral ossification also leads to the formation of two types of bone, compact and porous. Most bones are a mixture of both types, containing a compact outer surface and a porous interior.
The bones get constantly remodelled during our lives by the combined actions of osteoblasts laying down the new bone and osteoclasts, resorbing the bone tissue. This video tells you everything you need to know about osteoclasts. If you are a student or a young investigator first approaching the osteoclast field, take the opportunity to get to know what are the osteoclasts, how they differentiate, how they resorb bone and how their activity is altered in diseases. The video also describes the relationship between osteoclasts and other cells and the mechanisms regulating their function. You will be amazed by the great beauty of these cells.


